Leading Toward Justice in Healthcare
by David S. Williams III, co-Founder and CEO of Care3 and 2013 Henry Crown Fellow of The Aspen Institute

I had the absolute pleasure of attending The Aspen Institute's annual Action Forum last week in Aspen, CO. As the 1st inaugural Resnick Aspen Action Forum (thank you Resnick Family of The Wonderful Company!), the theme was bold: Leading Toward Justice.
The past 18 months have seen multiple shocking results within the criminal justice system with the deaths of unarmed black men at the hands of police and the subsequent lack of prosecution for these deaths. While the blame for these deaths face fierce debate in the community and the courtroom, justice can only be served when all people receive equal treatment under the law.
In what I and many attendees describe as the most powerful speech about injustice ever given, Bryan Stevenson, Executive Director of The Equal Justice Initiative brought an assembly of 400 global leaders to tears when describing the injustice he faces daily in his work with death row inmates. This speech is a MUST-SEE for anyone looking for ways to make meaningful change as he provides a four-point framework to lead toward justice.
- Get Proximate
- Change The Narratives that Maintain Injustice
- Stay Hopeful
- Be Uncomfortable
The Aspen Institute also posted a summary of Bryan's talk which, of course, doesn't do him "justice" on its own. Please watch the speech, listen, and feel what all of us in the room felt.
But injustice doesn't only apply to law enforcement and the criminal justice system in America. Think about our educational system and, most relevant to my professional work, the healthcare system.
Healthcare in America - Is Justice Served?
By any measure, the healthcare capabilities of US-based hospitals and health centers are the best in the world. With leading institutions such as Mayo Clinic, Cleveland Clinic, and many other healthcare systems, the knowledge of evidence-based care generated at these institutions gives US residents the opportunity to receive top-notch care.
Or does it?
Introducing the 2014 AHRQ National Healthcare Quality and Disparities Report. This annual scorecard measures different ways healthcare doesn't reach the "underserved" defined as the poor, people of color, the disabled, rural, and seniors. Across all measures of access, quality, and outcomes, underserved populations trail that of the general population. Is that justice?
For example, in one graphic AHRQ ranks each US state in quartiles by the quality of healthcare delivered:
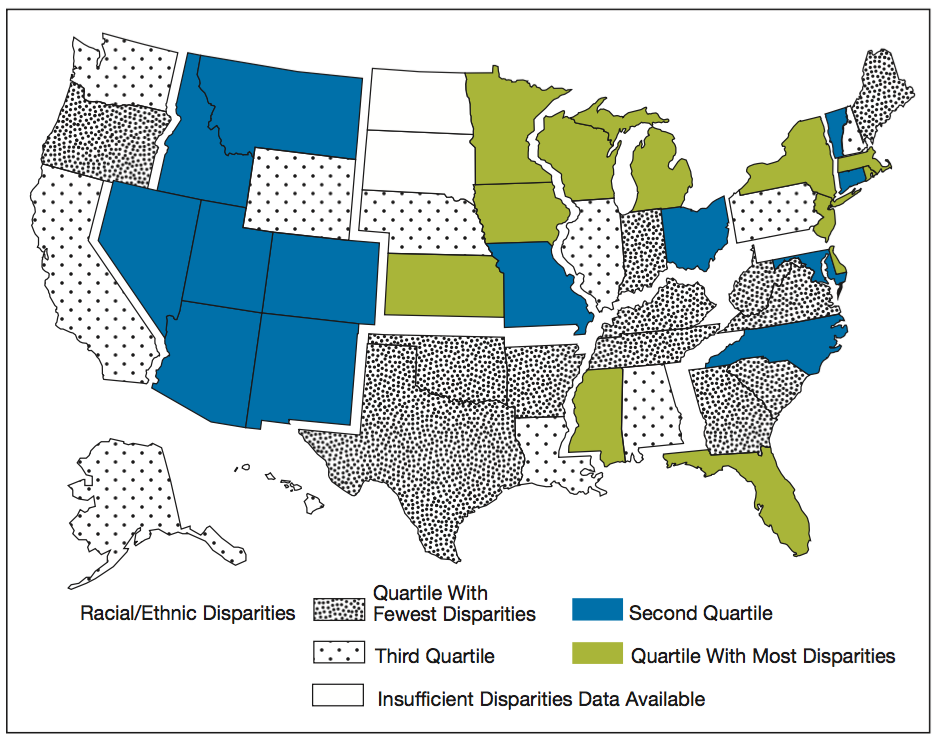
On a second graphic, AHRQ charts each US state by the level of disparity in healthcare delivered based solely on race:
(Note: A similar analysis was NOT completed in the 2015 AHRQ report)
An analysis of these charts (which AHRQ curiously didn't do themselves), one can see the states in which the highest level of care is delivered, while also having the highest level of disparity of care based on race. Six (6) states fall into that dubious group: Iowa, Wisconsin, Minnesota, Massachusetts, Rhode Island and Delaware (Michigan, Pennsylvania, NY and NJ are in the second highest quartile of quality, but also have the highest level of disparity).
Again, these six states have the capability to deliver the highest quality of care for their residents--but also sport the highest disparity levels of healthcare access, quality, and outcomes based solely on the race of patients.
Is this justice?
Further complicating this picture is a recent study by researchers at Johns Hopkins Medicine published in The BMJ (formerly British Medical Journal) stating that if medical errors were counted correctly, they would rank third on the list of causes of death in the US behind cardiovascular disease and cancer. The researchers penned an open letter to the CDC asking them to update their data collection methods to account for avoidable medical errors as a cause of death, not simply the underlying disease that led to the need for acute care. Their methodology in coming to that conclusion could also be applied to the environments in which healthcare disparities exist by race.
It doesn't take a scientist to recognize that a disproportionate level of medical errors likely occur to those in underserved populations. There is no accountability for avoidable medical errors in the same manner that (theoretically) the criminal justice system could apply accountability for broken laws because those medical errors are not counted.
If a disproportionate amount of the 250,000 suspected avoidable medical errors that lead to death in the US happen to patients in underserved populations because of poor quality being delivered, isn't that the same as unconscious bias (or perhaps conscious discrimination) leading to different treatment of people of color by law enforcement and the criminal justice system? Both groups have the capability of delivering better outcomes in the moment, but "somehow" the most optimal outcomes are not achieved.
Is that justice?
Healthcare providers do noble work. So do police officers. They are people we respect in our communities and need to perform at their highest levels to reach our best quality of life. Can we improve accountability and reporting to help increase quality and drive better outcomes for all? I believe we can.
Leading Toward Justice
Leading toward justice requires acknowledgement that injustice exists. Health disparities are a form of injustice and many organizations are standing up to research and fix the problem. These organizations have clearly identified the injustice in health disparities and are taking steps to eliminate them. Bravo.
Now it's time for action and results.
Care3 is built to battle inequities and disparities in healthcare using mobile and social technology. We welcome the opportunity to partner with healthcare entities such as hospital systems, health plans, community hospitals, and community-based care management firms in initiatives where measurable impact can be achieved with underserved populations.
About David S. Williams III
David S. Williams III is a leading innovator in consumer digital health. Care3 is inspired by David’s experience caring for his special needs son and the realization that the most vulnerable members of our society including seniors, people of color, and the disabled do not have equal access to healthcare and receive woefully inadequate quality of care in their homes and communities. Care3 is built to fix these unacceptable and unnecessary inequities.